Radiation-Induced High-Grade Spindle Cell Sarcoma Of The Sternomastoid Muscle - A Case Report
Learn about some of the complexities of high-grade spindle cell sarcoma. This rare cancer can still be treated, albeit it will take years to see favorable results.
Author:James PierceReviewer:Karan EmeryFeb 07, 2024361 Shares36.1K Views
How complex it could be to study the development and find treatment for high-grade spindle cell sarcoma?
Sarcomas developing as primary malignancies of the head and neck are a rare complication after radiation therapy. This kind of sarcoma has variable clinicopathological appearances and behavior.
Radiation-induced spindle cell rhabdomyosarcoma of the sternomastoid muscle is a very rare sarcoma and has very seldom been described in the literature.
Herein, we report on the development of a rapidly growing mass over the lateral side of the neck appearing after seven years in a patient with a history of laryngeal carcinoma who received radiotherapy and chemotherapy.
The process of diagnosis and management using combined surgery and targeted brachytherapy are discussed.
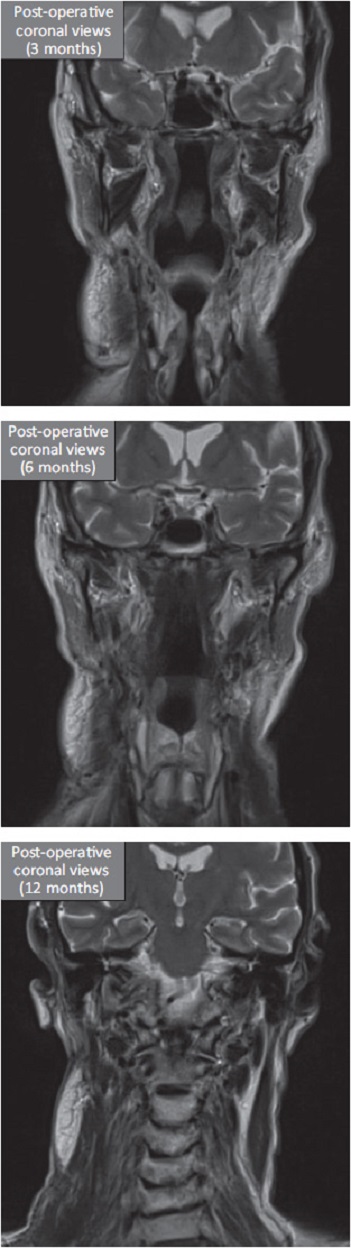
The patient experienced discomfort and oozing of the wound for up to two months after surgery; however, complete response with satisfactory adaptation and shrinkage of the pectoralis major pedicled muscle flap occurred after a year.
The patient has been disease-free for five years post-operation.
Radiation-induced spindle cell rhabdomyosarcoma of the sternomastoid muscle after treatment for laryngeal carcinoma may occur a long time after radiation therapy.
It can be clinically aggressive and radiographically distinctive and require multidisciplinary management.
Preliminary Discussion
Although radiotherapy is known to be an effective treatment modality in the management of malignant disease, ionizing radiation can also induce malignant tumor formation.
This has been shown by studies on the sequelae of human exposure to radiation from atomic testing.
The first recorded case of a radiation-induced cancer was a squamous cell carcinoma (SCC) that arose in the hand of a 33-year-old technician who had been testing roentgen tubes for four years.
Radiation-induced sarcoma (RIS) of the head and neck is a rare, long-term complication of treatment with radiotherapy.
Although there are many case reports on RIS in the medical literature, these cases cannot provide reliable information on the outcome of pathology as there are few reported series published with only a limited number of cases.
Post-irradiation sarcoma (PIS) is another name given to RIS.
The histological types include:
- angiosarcoma
- fibrosarcoma
- malignant schwannoma
- osteosarcoma
Spindle cell rhabdomyosarcoma (RMS) is a rare PIS first described in children in 1992 as a neoplasm composed mainly of fascicular spindle-shaped cells that show immunohistochemical and ultrastructural evidence of myogenic differentiation.
The etiology of spindle cell RMS in adults is unknown, with different subclasses. Radiation-induced RMS is a rare variant of this type of sarcoma.
The prognosis of patients with PIS is poor in general, regardless of the type and site, with most series reporting overall five-year survival rates of 10% to 30%.
The prognosis appears to be related to site, reflecting the feasibility of surgical resectability.
RIS of the extremities has the best prognosis. Those that have the worst prognosis are the areas in the body involving the:
- neck
- shoulder girdle
- pelvis
- vertebral column
Although adjuvant radiotherapy and/or chemotherapy have a role in the treatment of these tumors, the extent of adjuvant radiotherapy is limited by the amount of radiation previously received, leaving surgery as the only treatment option for most of these tumors.
However, using brachytherapy as an adjunctive to surgery to control residual sarcoma cells is a novel method.
To the best of our knowledge, no study has been conducted using this modality.
This report describes a case of adult spindle cell RMS in a patient who had previously undergone radiotherapy, treated by combined surgery and targeted radiotherapy (brachytherapy) with a follow-up for five years.
Case Report
A 67-year-old Caucasian male was referred to the Head and Neck Unit of University College London Hospital in London.
He was complaining of a painless lump in the right side of the neck, which had increased in size over seven months.
The mass did not cause any symptoms, including dysphagia or speech or breathing problems.
Past medical history included hypertension and hypothyroidism.
The patient was a non-smoker but chronic heavy drinker (40 units/week for over 20 years).
The patient was previously diagnosed with T3N0M0 laryngeal SCC seven years prior to his presentation to the unit. His treatment involved radiotherapy (66 Gy) and chemotherapy.
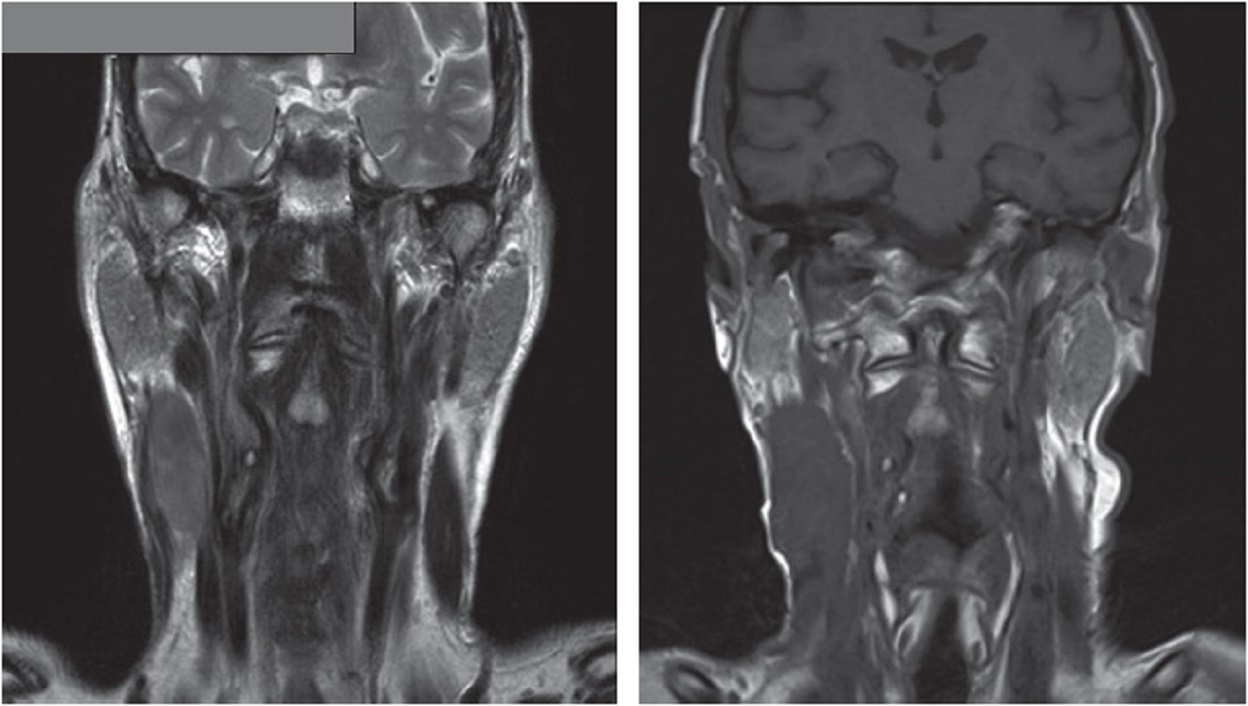
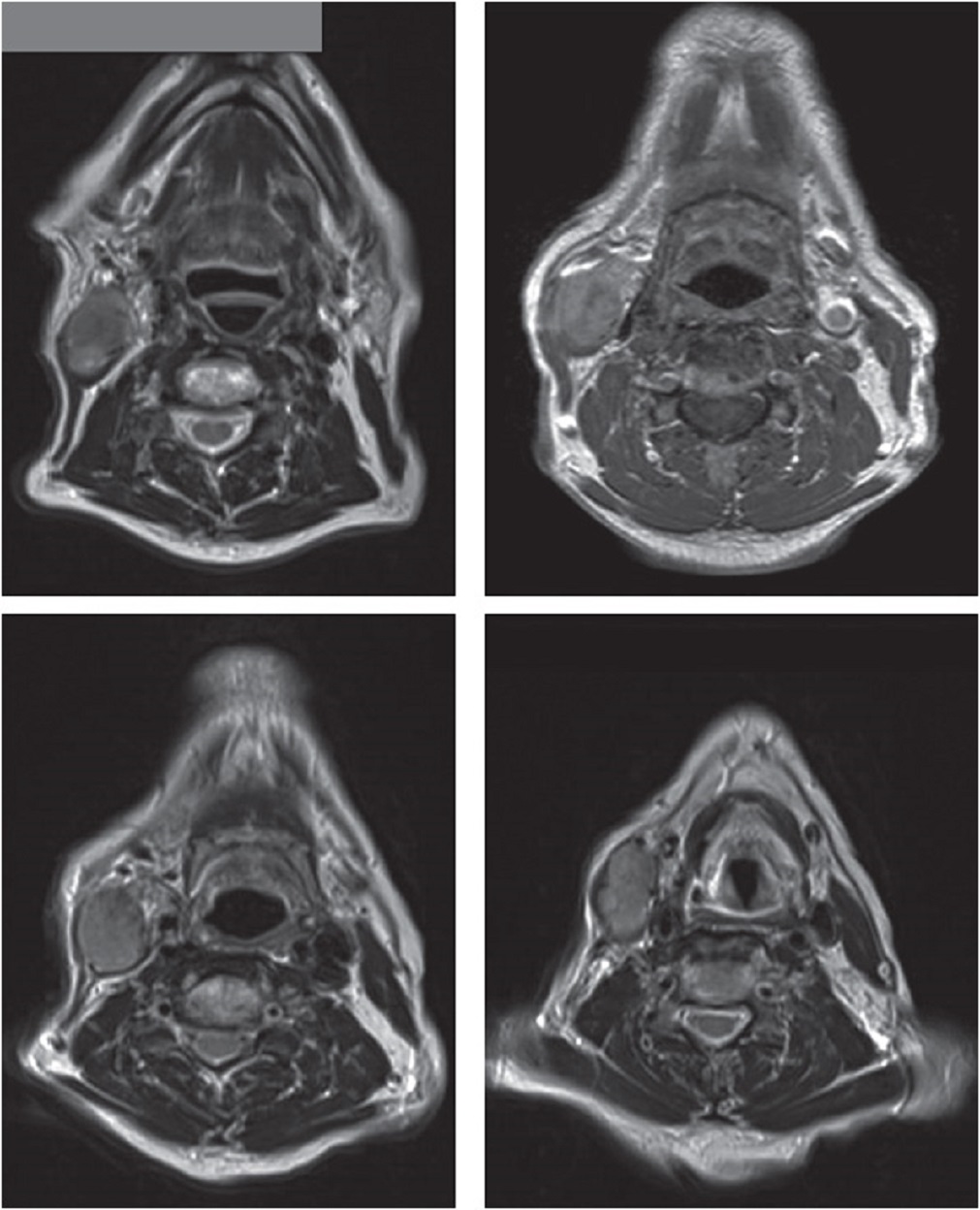
On clinical examination, the mass was 8 × 5 centimeters in size and infiltrated deep into the sternomastoid muscle.
There were no palpable lymph nodes.
Magnetic resonance imaging (MRI) of the neck reported a fixed solitary mass in the right neck (levels II and III) arising from the sternomastoid muscle, with heterogeneous high signal intensity on T2-weighted images and low signal intensity on T1-weighted images.
The patient was examined under anesthesia that confirmed the findings.
The endoscopic examination of the oropharynx and larynx was unremarkable.
After an ultrasound-guided core biopsy, the diagnosis was confirmed histopathologically as radiation-induced high-grade spindle cell sarcoma.
Agreement on the Multi-Discipline Meeting (MDT) was reached and the patient received single-agent doxorubicin for three cycles.
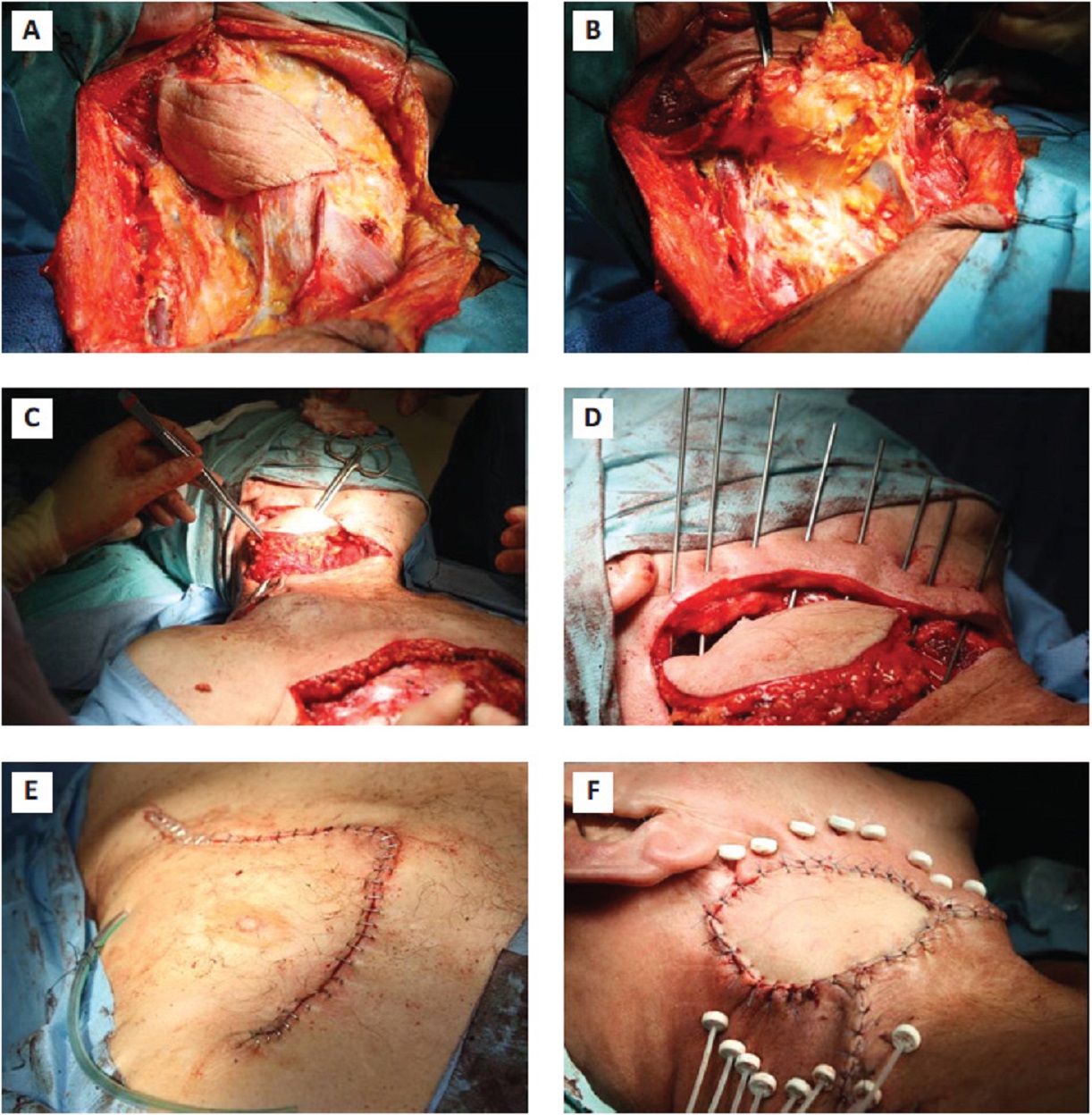
This was followed with extended radical neck dissection with clear margins, which was successfully performed.
It was followed by reconstruction with an ipsilateral pectoralis major pedicled muscle flap and insertion of brachytherapy catheters.
Recovery after anesthesia was uneventful.
The patient complained of discomfort in the area of surgery, with clear fluid discharge from the chest (flap donor area) for up to two months, which healed later with simple conservative dressings.
Macroscopically, a well-circumscribed but not encapsulated, solid, solitary red lesion was encased in thick fibromuscular tissue.
Microscopic examination revealed:
- elongated, spindle-shaped cells with vesicular nuclei
- numerous mitoses
- a pale cytoplasm forming long fascicles
These cells were mixed with sparse polygonal or rounded rhabdomyoblasts, with foci of sarcomeric differentiation.
Immunohistological staining was positive for desmin, which confirmed the myogenic nature.
Radiation was given twice daily for three consecutive weeks. The patient had an uneventful recovery and remained disease-free at his 5-year follow-up.
Main Discussion
RMS is a malignant mesenchymal tumor that originates from immature cells which are destined to differentiate into striated skeletal muscle.
RMS predominantly affects children, constituting >50% of all pediatric soft tissue sarcomas. It can be subdivided into three histological subtypes:
- embryonal
- alveolar
- alveolar
Spindle cell RMS is a less common variant of embryonal RMS and is predominantly composed of spindle cells.
The tumor is most often encountered in the paratesticular region in children, in whom it is generally associated with a better prognosis.
The first two cases of spindle cell RMS in adults were described in a study published in the journal in The American Journal of Surgical Pathologyin 1998.
Little is known about the etiology of spindle cell RMS in adults.
In this study, RIS developed in this patient, although radiotherapy was effective in the management of a malignant tumor of the larynx.
Determination of a cause-effect relationship between prior irradiation and radiation-induced tumor formation requires the following criteria:
1. documented history of irradiation in this site
2. the new malignancy must arise within the irradiated field
3. the new tumor must be histologically distinct from the original primary lesion
4. the latent period between irradiation exposure and development of the new malignancy must be five years or longer
Our patient fulfilled the criteria by virtue of the tumor’s location, previous and new histology and latency period of more than years.
The presenting signs and symptoms of radiation-induced RMS are variable, depending on the:
- site of initial presentation
- extent of the tumor
- presence or absence of distant metastases
- lymph node involvement
Patients generally present with a fast-growing mass.
Diagnosis is difficult because of induration and fibrosis of the tissue within the former field of radiation.
Generally, RISs are associated with an outcome significantly poorer than that of stage-matched soft tissue and osteogenic sarcomas that arise independently of irradiation.
The 5-year disease-free survival rate for RIS is 10% to 30%.
The poor prognosis of RIS in the head and neck region may be explained by the following factors:
a. delay in diagnosis
b. proximity of the tumor to major neurovascular structures, which may place constraints on the limits of surgical resection
c. limited treatment options because of the dangers of irradiating the previously irradiated field and the relatively poor sensitivity of these tumors to chemotherapy
d. RIS in the head and neck may be biologically more aggressive
e. RIS develops from radio-resistant tumor clones and may not be responsive to further radiotherapy
Early detection is the main hope for survival in RIS cases because there are no preventive measures to safeguard patients with cancer against RIS apart from limiting radiotherapy or using surgery as the primary treatment modality.
Thus, immediate workup should be performed when any pain or swelling occurs in an irradiated field - the clinical diagnosis of RIS can be difficult due to fibrosis and induration within the irradiated field.
The management of RIS is challenging and differs from that of sarcoma not induced by radiation.
Complete surgical excision appears to offer the best means of palliation and the only rational chance for long-term survival.
Prognosis is related to the site and resectability; thus, RIS of the extremities has a 5-year cure rate of 30% whereas RIS of the vertebral column and pelvis is associated with a 5-year survival rate of less than 5%.
The survival rate of RIS in the head and neck is somewhere in between these rates. In our patient, critical anatomy at the lymph node neck levels II and III did not limit us in obtaining a wide surgical margin.
Although only limited follow-up data are available, adult spindle cell RMS appears to have a more aggressive clinical course when compared with cases occurring in the pediatric population.
Experience with treatment of adult spindle cell RMS is limited.
Treatment options include surgery, radiation therapy and chemotherapy.
Patients are categorized according to their risk assessment, using a clinical group and a site-based tumor-nodes-metastasis staging system.
Conclusion
Despite poor prognosis and aggressive pattern of such a rare kind of sarcoma, combining surgery with brachytherapy achieved a disease-free survival for five years.
Brachytherapy has several advantages, including delivering a higher dose of radiation to the tumor while minimizing exposure to surrounding healthy tissues.
Along with surgery, this form of radiation therapy aims to treat high-grade spindle cell sarcoma.

James Pierce
Author

Karan Emery
Reviewer
Latest Articles
Popular Articles