Post-Polio Syndrome - How It Relates To Dysphonia
Post-polio syndrome is a condition that manifests itself in polio survivors long after they have fully recovered from the initial infection with the polio virus that caused the disease. It is a condition that evolves into a more serious one over time. Post-polio syndrome is characterized by a collection of symptoms that, taken together, make it challenging for patients to lead independent lives and, more broadly, to experience happiness.
Author:James PierceReviewer:Karan EmeryAug 30, 20225 Shares343 Views

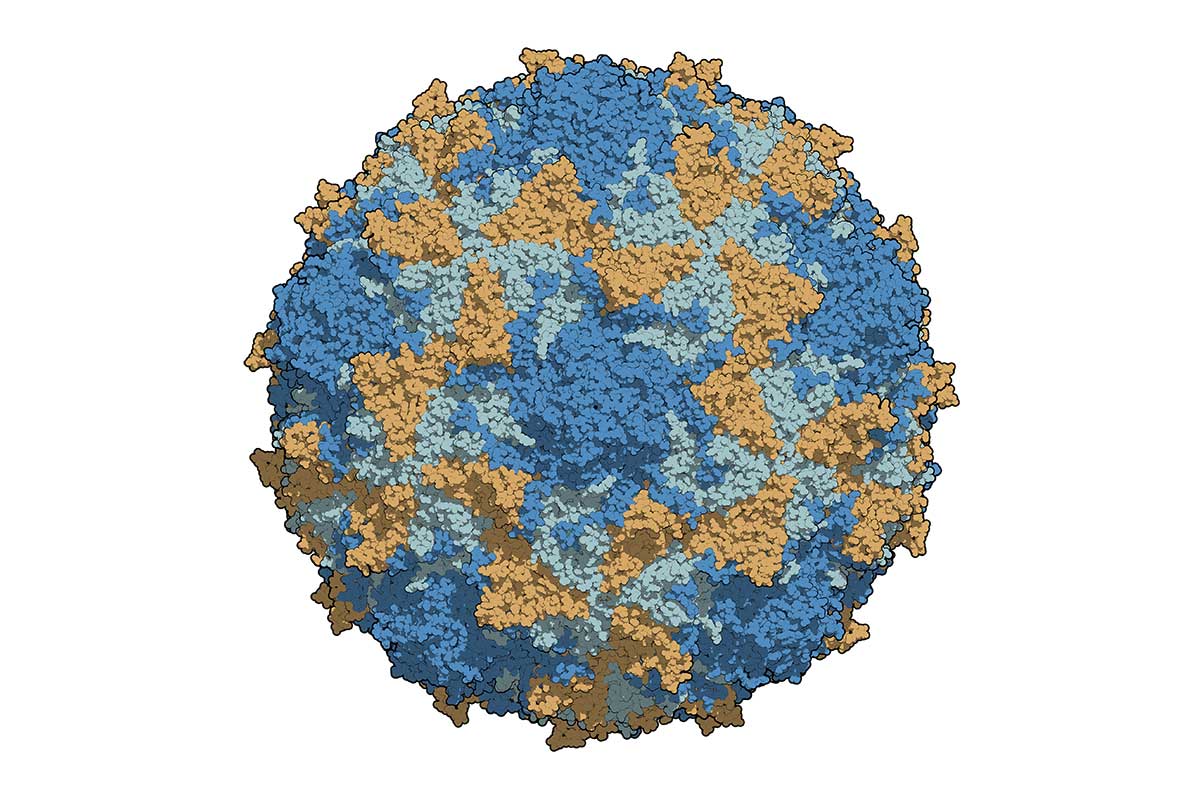
Post-polio syndromeis a condition that manifests itself in polio survivors long after they have fully recovered from the initial infection with the polio virus that caused the disease.
It is a condition that evolves into a more serious one over time.
Post-polio syndrome is characterized by a collection of symptoms that, taken together, make it challenging for patients to lead independent lives and, more broadly, to experience happiness.
Among these symptoms include general exhaustion, pain, difficulty breathing, depression, and inability to sleep.
Dysphonia, which is more widely known as hoarseness, may be the cause of your voice becoming raspy or husky.
Perhaps you were talking too loudly in a crowded restaurant, or perhaps there is an underlying medical problem that is the cause of this symptom.
The hoarseness that you are experiencing should go away after a short period of time; however, if it continues for three weeks or longer, you should consult a medical professional.
An interesting instance of dysphonia in a patient with post-polio syndrome is presented in this article.
What Is Post-Polio Syndrome?
Post-polio syndrome is characterized by a gradual loss of muscle strength 15–30 years after the first polio infection in polio patients who have survived the disease.
It weakens not only the muscles that were initially afflicted by the poliomyelitis virus but also the muscles that are surrounding those that were not initially impacted by the virus.
It is possible to interpret it as an adversary who is assaulting deceptively and does not disclose themselves all at once.
It gradually worsens a person's physical circumstances, with occasional periods of stability in between, which makes it difficult to recognize the rapidly deteriorating condition immediately.
The effect of PPS could make it difficult for a person to carry out the activities that make up his or her typical day.
In its most severe manifestation, PPS can make it difficult for a person to both swallow and breathe normally.
Although it might make life a living nightmare, most of the time it does not pose a threat to one's life... PPS was only rarely the cause of someone's death.
Poliomyelitis or polio, Causes, Signs and Symptoms, Diagnosis and Treatment.
What Causes Post-Polio Syndrome?
To tell you the truth, modern medical research has not been successful in identifying the factors that contribute to post-polio syndrome.
A number of researchers have made attempts to provide a theoretical explanation; nevertheless, none of them have been successful in putting forth the real fact.
Accordingly, the actual cause of PPS has not been identified to this day.
However, over time, one of the hypotheses emerged as the clear frontrunner in terms of support.
According to this theory, the muscle weakness caused by PPS may be the result of degeneration of individual nerve terminals in the motor units that have remained after the original polio illness.
This theory is based on the speculation that these nerve terminals may have become damaged as a result of polio.
How Is Post-Polio Syndrome Diagnosed?
It's possible that by now you've already figured out that the field of medical science knows very little about this physically deceptive ailment.
They don't know what causes post-polio syndrome (PPS), and they don't have a test that can identify it either.
How exactly can one determine whether or not they have developed post-polio syndrome?
Unfortunately, only a small percentage of doctors are able to detect PPS, and those that are would do so through a system of trial and error.
The medical history of the patient would be thoroughly examined first, and it would be determined whether or not the patient had polio as a child.
After that, the patient would have to go through a series of tests and neuromuscular examinations so that the doctor can rule out other illnesses and conditions that may cause symptoms that are similar to those being presented by the patient.
For instance, a patient may be given tests to see whether or not they are suffering from depression.
This is because sadness can produce unexplained fatigue, which is a symptom of PPS.
After ruling out all other possible illnesses and conditions, medical professionals are able to arrive at the conclusion that the patient has developed PPS.
You might be wondering why you should visit the doctor if they are unable to provide an accurate diagnosis of PPS.
In the event that you notice the symptoms of PPS, there is a very straightforward justification for seeking medical attention from a specialist in neuromuscular illnesses.
The majority of the other conditions that might create symptoms that are identical to those of PPS are treated.
Therefore, if the symptoms you're experiencing are attributable to a condition other than PPS, you might be cured!
What Are The Symptoms Of Post-Polio Syndrome?
Fatigue is the primary indicator of post-polio syndrome (PPS).
Without having engaged in any particularly taxing activity, a person will begin to experience feelings of fatigue.
Other symptoms that may be indicative of post-polio syndrome include the following:
- Lowered resistance to the effects of cold temperatures.
- A disruption in the natural cycle of sleep as well as trouble breathing when sleeping.
- Atrophy of the muscles.
- Escalating difficulties with both breathing and swallowing.
- Skeletal abnormalities like scoliosis.
- Body aches and pains in the joints.
- Muscle and joint weakness that gradually spreads throughout the body.
The 4 Underlying Causes of a Hoarse Voice
What Is Dysphonia?
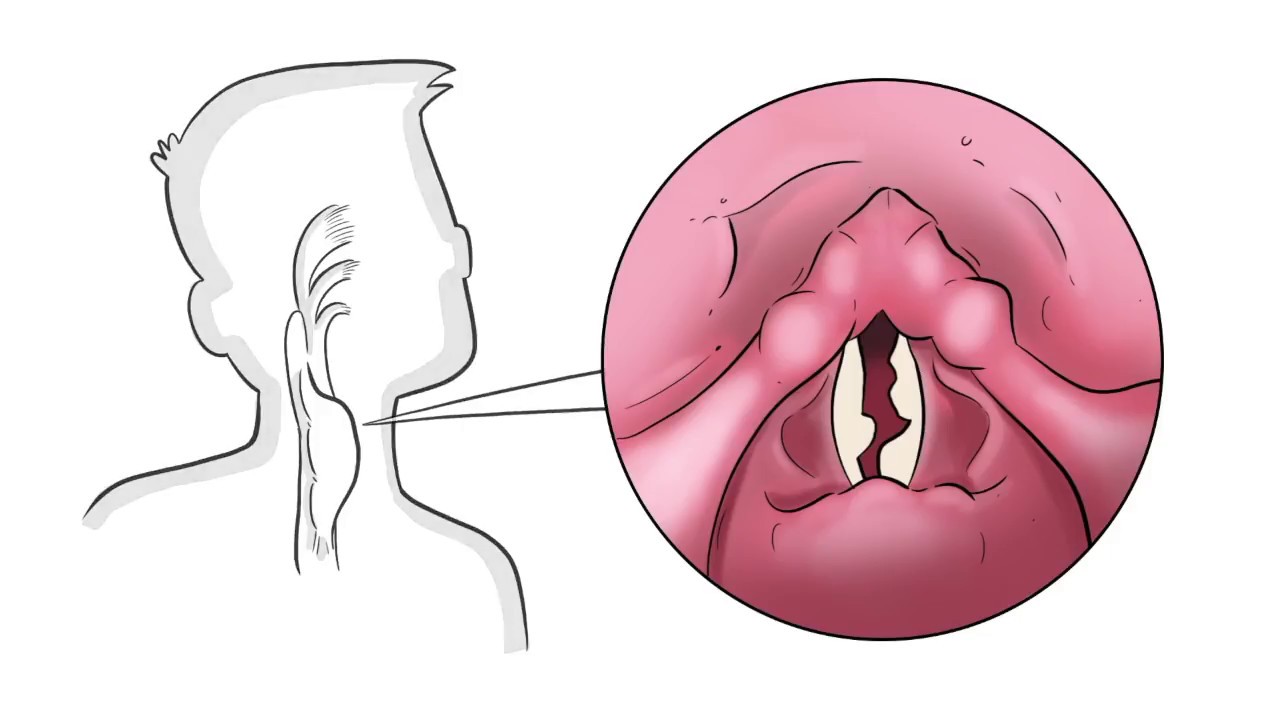
Dysphonia, often known as hoarseness, is a condition in which a person's voice becomes raspy, strained, or breathy.
Both the loudness and the pitch may be altered to some degree.
There are numerous factors that can lead to hoarseness; however, the good news is that the majority of these factors are not life-threatening and typically resolve themselves in a short period of time.
It's not uncommon to have a hoarse voice. It is estimated that approximately one-third of people will have it at some point in their lives.
Hoarseness is a condition that can affect people of any age.
This symptom is more prevalent in those who smoke and in those who make a living using their voices professionally, such as lecturers, singers, sales representatives, and people who work in call centers.
What Causes Dysphonia?
There are a number of different potential causes of dysphonia. Many are completely safe. Causes include:
- Tension dysphonia. Muscular tension dysphonia is a change in voice sound or feel caused by muscle tension in and around the voice box. This stress hinders your voice. Muscle tension dysphonia can develop during laryngitis and persist after vocal cord edema subsides. Stress and other situations might induce it.
- Rhinopharyngitis (RRP/laryngeal papillomatosis) recurrence. Noncancerous tumors line the airways in patients with this condition.
- Cancer of the larynx. In some cases, laryngeal cancer might manifest as a persistent hoarseness that lasts for longer than a few weeks.
- Paralysis of the vocal folds. As a result, one or both of your vocal cords are paralyzed. There is a chance that one or both of the doors will not open or close. In most cases, there is no known cause, however it can occur as a result of an injury, cancer of the lung or thyroid, infection, MS, stroke, Parkinson's disease, or tumors.
- Cysts, polyps, and nodules of the vocal cords are all possibilities. It is possible to develop nodules, polyps and cysts on your vocal folds, all of which are non-cancerous. Because of excessive friction or pressure, they develop.
- Neurological diseases and conditions. If you've had a stroke or Parkinson's disease, your illness may have affected the part of your brain that controls the muscles in your larynx.
- Bleeding in the vocal folds. If you lose your voice suddenly or can talk but not sing, you may have had a vocal fold hemorrhage. This happens when a blood vessel on a vocal fold breaks and lets blood into the muscles.
- Gastroesophageal reflux (GERD) (GERD). GERD is also called "heartburn" because stomach acid goes up into the throat. Laryngopharyngeal reflux happens when the acid goes all the way up to your vocal folds (LPR).
- Laryngitis. This happens when allergies, a cold, or an upper respiratory infection make your vocal folds temporarily swell.
- A cold or infection in the sinuses.
- You're talking too much. You might get hoarse if you talk too long, cheer too loudly, sing too much, or speak in a higher or lower pitch than usual. Also, as you get older, your vocal cords get thin and floppy. As you get older, it's normal for your voice to get rougher.
Case Presentation
The patient is a male who is sixty years old and was diagnosed with post-polio syndrome in an outpatient rehabilitation post-polio clinic at a tertiary academic institution.
The clinic specializes in treating patients who have been affected by polio.
The patient's principal issue was that they had a hoarse voice when they came in for their appointment.
The patient developed a direct functional handicap as a direct result of the illness since the patient worked as a teacher and found it difficult to complete a full day of instruction while suffering from dysphonia.
As a result of the condition, the patient developed a functional handicap.
As a consequence of the difficulties, he was under the assumption that he would no longer be able to continue working in this field.
There was a history of cancer of the vocal cords in the patient's family, and the patient themselves had a history of vocal cord polyp.
He became infected with polio in 1950, which left him with significant residual weakness in his right leg.
Because of this, he was forced to make long-term use of a KAFO in conjunction with bilateral axillary crutches.
Following days that were especially challenging for him, he would also suffer from tremendous tiredness.
The patient was evaluated concurrently by a physiatrist, a physical therapist, and an orthotist.
All three of these specialists are specialists in the field of medicine.
During the otolaryngology examination, it was discovered that the vocal cords had a range of motion that was normal for them.
It was found that stomach problems were not the root cause of the hoarseness.
The chest CT came back without any significant findings.
The speech pathologist came to the conclusion that the hoarseness was caused by weary abdominal muscles that were weakened due to post-polio syndrome.
This led to hoarseness. There was a discernible improvement in the patient's voice function after the introduction of speech therapy for energy conservation strategies and physical treatment to strengthen the belly and core muscles.
Both of these treatments were concurrent with the patient's treatment.
It was recommended that the patient wear an abdominal binder 24 hours a day in order to offer support for the abdominal and diaphragmatic musculature.
What You Should Know About Post-Polio Syndrome
However, this patient's instance shows an unusual relationship between hoarseness and weakness, which is a common post-polio syndrome symptom.
It's possible for people who've had polio in the past to acquire post-polio syndrome, which is characterized by symptoms such as weakness, pain, and weariness returning at a later date.
Post-polio syndrome affects between 22 and 68 percent of polio survivors. There is a danger of muscle weakness for everybody who has ever had polio, regardless of how severe their episode was.
A larger loss of muscle function is more prevalent in those who had severe residual weakness following their first polio infection.
This is known as post-polio syndrome. In addition, they are more likely to suffer from post-polio ataxia.
Although non-fatiguing exercise, energy conservation measures, and suitable bracing or assistive equipment have been shown to be the most effective treatments for post-polio syndrome, in certain people even minimal physical activity may increase post-polio syndrome symptoms, such as weariness.
Post-polio syndrome cannot be cured because there is no effective treatment or preventive at this time.
People Also Ask
Is Post-Polio Syndrome A Disability?
As a result of post-polio syndrome, an individual's work and personal life may be adversely affected. Post-polio Syndrome can make you ineligible for Social Security Disability benefits if it prevents you from working.
Can Post-Polio Syndrome Affect The Heart?
Everyone is susceptible to neuromuscular disorders (NMDs), which can strike at any time and without warning. Disabilities and reduced quality of life can be caused by muscle weakness that affects breathing, coughing and swallowing as well as speech and limb muscles.
What Is The Treatment For Post-Polio Syndrome?
The following treatments may help alleviate your post-polio syndrome symptoms: Conservation of energy. Pacing yourself and taking frequent breaks will help you avoid exhaustion. The use of assistive devices (such as a cane, walker, wheelchair, or a motor scooter) can help you save energy.
Does Post-Polio Syndrome Affect Memory?
The exhaustion caused by post-polio syndrome also has a negative effect on mental health. Patients often use the term "brain weariness" to describe difficulties in the areas of attention, focus, memory, and clarity of thought. Cognitive tiredness in individuals with PPS is a topic that has received less attention thus far.
Conclusion
It's critical that you take care of your voice because it's one of your most valuable instruments for communicating.
Hoarseness can be irritating or distressing if you work with your voice.
If you have to talk loudly, take good care of your voice by drinking enough of water, avoiding caffeine, and quitting smoking.
You can also use a microphone or other amplification device.
Patients with post-polio syndrome who are suffering hoarseness in their voice can benefit from a multidisciplinary team.
If you've had polio in the past, you should be checked for abdominal, diaphragmatic, and laryngeal muscular weakness.
If the hoarseness persists for more than three weeks, visit your doctor.

James Pierce
Author

Karan Emery
Reviewer
Latest Articles
Popular Articles