Microglia In Neurological Diseases - Effective Use For Brain Disease Inflammation
We will look at the function of microglia in neurological diseases including Parkinson's, Alzheimer's, and FTD, where microglial activation is linked to the development of the illness and the severity of the symptoms. Depending on the anatomical region, microglia make about 0.5-16.6% of the total cell population in the human brain and 5-12% in the mouse brain.
Author:Karan EmeryReviewer:James PierceOct 12, 202240 Shares1K Views
We will look at the function of microglia in neurological diseases including Parkinson's, Alzheimer's, and FTD, where microglial activation is linked to the development of the illness and the severity of the symptoms.
Depending on the anatomical region, microglia make about 0.5-16.6% of the total cell population in the human brain and 5-12% in the mouse brain.
The quantity and operation of microglia are tightly regulated by the local microenvironment and cell-cell interactions in physiological situations.
In response to an injury, microglia may change their morphology (i.e., shorter processes), phagocytic activity, antigen presentation, and release of inflammatory chemicals including cytokines and chemokines.
The local microenvironment and disease settings, where microglia intimately interact with neurons, astrocytes, and oligodendrocytes, differ across the several illnesses displayed in the different locales.
As a result, the microglial phenotype is disease-specific and may be modified by factors such as biochemical and cellular composition, neuronal subpopulations and circuits, neurotransmitters, and the local metabolic rate.
What Is The Definition Of Neurological Disease?
The World Health Organisation (WHO), defines neurological disorders as illnesses of the nervous system, both in the brain and in the body's extremities. Meaning the central nervous system (CNS), autonomic nervous system (ANS), neuromuscular junction (NMJ), and muscles.
A wide range of neurological conditions are included in this category: epilepsy (including Alzheimer disease and other dementias), cerebrovascular diseases (such as stroke), migraine (and other headache disorders), multiple sclerosis (MS), Parkinson's disease, and neuroinfections (such as encephalitis and meningitis).
The nervous system can be affected by a wide range of infections, including bacterial (such as Mycobacterium tuberculosis and Neisseria meningitides), viral (such as HIV, enteroviruses, West Nile virus, and Zika), fungal (such as Cryptococcus and Aspergillus) and parasitic (such as malaria and Chagas). Neurological symptoms may be caused by the virus itself, or by the body's immune system.
Neurological problems impact hundreds of millions of individuals across the globe. Over 80 percent of stroke fatalities occur in low and middle-income countries, with more than 6 million deaths occurring each year.
Epilepsy affects more than 50 million individuals globally. Alzheimer's disease is the most frequent form of dementia and may be responsible for 60–70% of all cases. There are an estimated 47.5 million individuals worldwide with dementia and 7.7 million new cases per year.
According to the World Health Organization (WHO), nearly one in 10 people suffers from migraines.
What Is A Microglia?
This network of cells spans the whole brain parenchyma and is made up of microglia, the central nervous system's innate immune cells. During the first trimester of pregnancy, the yolk sac has a distinct stem cell population that gives rise to murine microglia.
At an early stage in fetal development, before brain vasculature arborization is complete and the blood–brain barrier (BBB) is entirely established, microglial progenitors move and populate the brain. This long-lived cell population of microglia is limited to the adult brain by the completely established BBB and is able to divide and self-renew over the course of one's life.
Using pharmacological inhibition of the colony-stimulating factor 1 receptor, mature microglia were eliminated in a recent research. They discovered that microglia quickly recovered their resilience once the inhibitor was removed, most likely from an in situ progenitor population.
Alzheimer’s Disease Pathology
The etiology and the underlying causes of Alzheimer's disease (AD), the most widespread kind of dementia caused by neuronal loss, are still not fully known. AD is characterized by a loss of neurons in the brain.
Both an abnormal intraneuronal buildup of hyperphosphorylated tau protein and an excessive synthesis and/or lack of clearance of amyloid-β (Aβ) peptides produced from APP cleavage have been implicated in the extracellular deposition of amyloid-β (Aβ) plaques in Alzheimer's disease.
Amyloid-beta plaques are found in the brains of people with Alzheimer's disease. Microtubules are kept in order by normal tau, but under pathological conditions, an accumulation of hyperphosphorylated tau occurs inside the cell, which leads to microtubule disorganization. This has been linked to neurodegeneration as well as a reduction in cognitive function.
The etiology of Alzheimer's disease might cause it to be categorized as either a familial or an idiopathic illness. People under the age of 65 who are diagnosed with early-onset Alzheimer's disease nearly invariably have a genetic form of the condition.
In many cases, a single mutation in the APP, presenilin 1 (PSEN1), or presenilin 2 (PSEN2) genes is to blame for the illness (PSEN2). Around ninety percent of persons who have Alzheimer's disease are believed to have a multifactorial component to their condition, which is a component of the illness that is assumed to be caused by variables such as heredity, environment, and lifestyle.
Alzheimer's disease is associated with a high level of activation of the innate immune system, which suggests that neuroinflammation is a significant factor in the development of Alzheimer's disease. In genome-wide association studies, more than 20 genetic loci have been identified as having a significant relationship with the chance of developing Alzheimer's disease and microglial immune responses (GWAS).
Activation Of Microglia In Alzheimer’s Disease
It is expected that the hippocampus will experience both functional and structural changes as Alzheimer's disease progresses throughout the course of its lifetime.
As was mentioned before, PRRs are able to bind to a wide variety of DAMPs and PAMPs. Microglial cells, for example, are susceptible to inflammation when Aβ species are present. The amyloid-like structures that bacteria and other microorganisms create constitute the first line of defense for the innate immune system in the brain.
In light of this, the microglial response to A may have developed in this manner as a result of evolution. Inflammasomes, toll-like receptors (TLRs), and apolipoprotein E (ApoE) are just a few examples of the significant risk factors that are related with PRRs that will be discussed in the next section.
The ApoE protein is responsible for regulating both the metabolism of the cell as well as the transport of fat. There have been shown to be four unique alleles of the ApoE gene. The risk of Alzheimer's disease increases by a factor of three to eight when there are three to eight copies of the ApoE 4 allele in the genome.
It is likely that the rare ApoE 2 allele may provide protection against Alzheimer's disease, in contrast to the more frequent ApoE 3 allele, which seems to have no impact, and the ApoE 4 variant, which offers a significant risk for developing the illness.
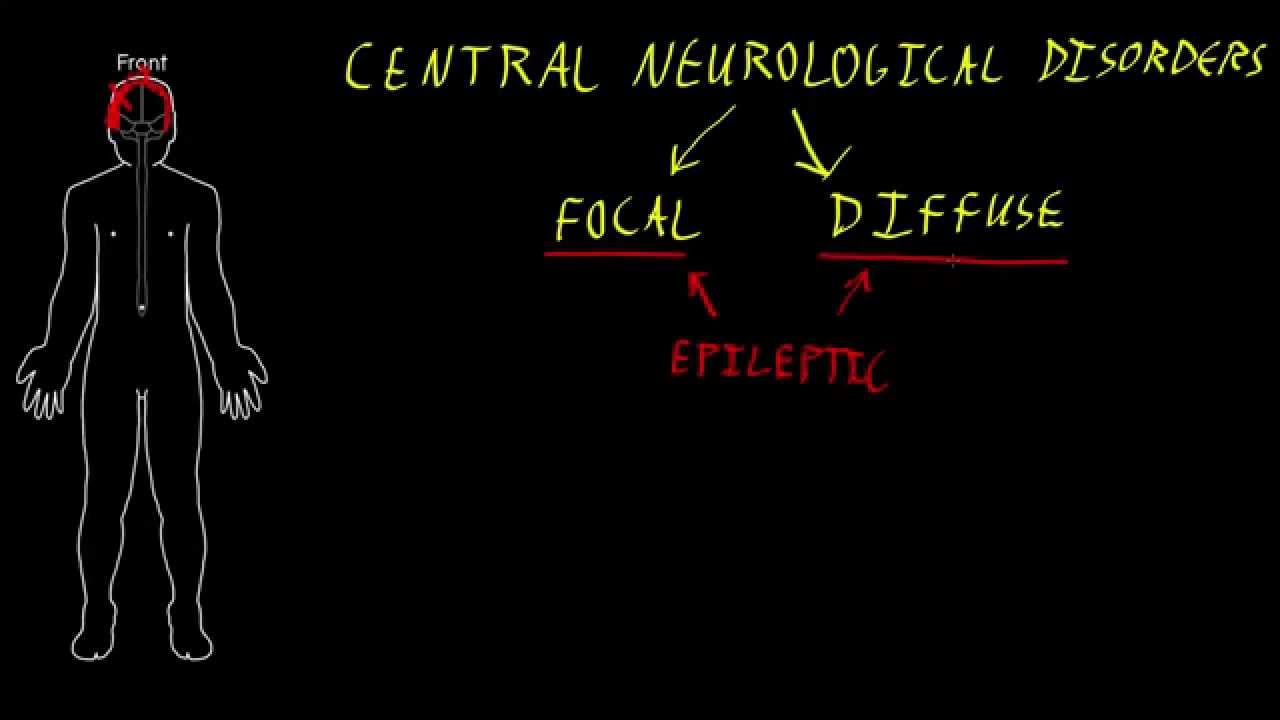
Central neurological disorders
Frontotemporal Dementia
The loss of cortical and subcortical capacities is a hallmark of frontotemporal dementia (FTD), which may be either permanent or progressive. This is the most common form of early-onset dementia and the third most common kind of dementia overall, after Alzheimer's disease (AD) and dementia with Lewy bodies (DLB).
Cognitive impairment, as well as irregularities in mood, behavior, and personality, are all symptoms that are associated with frontotemporal lobar dementia. This kind of dementia is caused by neuronal loss, gliosis, and microvascular alterations in the frontal and temporal lobes (FTLD).
There are three different types of FTLD, and each one focuses on a different protein component of abnormal neuronal and glial deposition and distribution. These three types are as follows: The majority of cases of FTLD are known as FTLD-Tau, which is linked to the microtubule-associated protein Tau.
This is followed by FTLD-TDP, which is linked to the 43 kDa transactive response DNA-binding protein, and finally by the extremely rare FTLD-FUS, which only occurs in approximately ∼5% of cases.
Activation Of Microglia In Frontotemporal Dementia
According to a number of studies that were published not too long ago, alterations in neuroinflammation and protein aggregation could already be present in the early stages of FTLD or AD.
Enhanced binding of the microglial ligand 11-C-R-PK1195 to frontotemporal brain regions in PET imaging studies demonstrates that microglial activation may begin at the early stages of FTLD. This finding lends credence to the hypothesis that microglial activation may occur at this point.
Alzheimer's disease patients have been shown to have activated microglia in their brains, which has been associated with cognitive decline (AD).
The patterns of microglial activation that are seen in FTLD and AD are congruent with the pathophysiology of the diseases. As a consequence of this, the level of microglial activity in the frontal subcortical white matter of patients with FTLD is higher, but in the temporal regions of AD patients, it is more apparent.
At the molecular level, the familial form of Alzheimer's disease (FTLD) and many genes connected to microglial activation have been linked to each other.
Parkinson’s Disease
Parkinson's disease (PD), a disorder of the motor brain characterized by the death of dopaminergic neurons, is the leading cause of increasing movement impairment. The neuroinflammatory response seems to have a role in the progression of Parkinson's disease, as shown by the findings of a number of studies that investigated the innate immune response in Parkinson's disease.
The Locus Coeruleus (LC) is another significant component in the pathophysiology of Parkinson's disease, which is a topic that will be covered in further detail in the next section.
People who have Parkinson's disease often experience a loss of dopaminergic neurons in the SNpc. When these neurons leave the SNpc, their axons go to the striatum, where they are received. Movement problems are a common symptom of Parkinson's disease, which is caused primarily by the destruction of neuronal connections in affected areas of the body.
Other regions of the brain, such as the LC (dorsal motoneurons), the amygdala, and the hypothalamus, all experience a loss of dopaminergic neurons as a consequence of this. Another characteristic feature of the illness is the presence of intraneuronal aggregates of misfolded α-synuclein, which are referred to as Lewy bodies.
These inclusions may be seen in both neuronal somas (also known as Lewy's bodies, or LB) and neurites (also known as Lewy's neurites). Even though α-synuclein inclusions are a hallmark of Parkinson's disease, it is possible to find them in other disorders as well, such as dementia with lewy bodies (DLB).
Activation Of Microglia In Parkinson’s Disease
In addition to the death of dopaminergic neurons in the SNpc and the accumulation of intraneuronal synuclein, inflammation plays an essential part in the progression of Parkinson's disease.
In the spinal nodes of the brain, an abnormally high number of microglia may be seen (SNpc). In Parkinson's disease, both microglia and astrocytes contribute to the inflammatory response, albeit only to a limited extent. In the introduction, we said that microglial cells play a role in the process of clearing away debris associated with the degeneration of neurons.
Inflammatory substances such as pro-inflammatory cytokines, chemokines, and reactive oxygen and nitrogen species (ROS and RNS) may be produced as a result of the activation of microglia by death cell debris. Microglia can be triggered by death cell debris (RNS). As a direct consequence of this, it is probable that neuroinflammatory responses have a role in the progression of the illness.
Directions For The Future
There is compelling evidence that the innate immune system and the response of microglia play a role in the course of neurodegenerative disorders such as Parkinson's disease and Alzheimer's disease.
Microglial cells are able to undergo a variety of functional activation states, which allows them to play an active role in maintaining brain homeostasis. On the other hand, a negative consequence might be reached if the inflammatory response caused by microglial cells is not well managed.
Molecule such as TNF-α, IL-1β, and iNOS are the primary outcomes of the downstream signaling of these pathways. The JAK/STATs and NFkB pathways are primarily responsible for governing the microglial pro-inflammatory response. This activation is connected to a detrimental effect in neurodegenerative illnesses, enhancing the inflammatory response and increasing the amount of neuronal damage that occurs as a result.
People Also Ask
Which Is The Best Description Of The Function Of Microglia?
It was unknown for a long time how microglia functioned. Today, it is understood that these cells serve as macrophages to eliminate cellular debris and dead neurons from brain tissue via the process of phagocytosis, mediating immunological responses in the central nervous system (cell eating).
Why Are Microglial Cells Important?
The central nervous system has a particular population of macrophages known as microglial cells (CNS). They are crucial for preserving the CNS's health since they get rid of infections and damaged neurons.
How Do Microglia Contribute To Sensation Of Pain In The Brain?
The quick onset of pain is another notable distinction between it and other neurological disorders. Microglia control neuronal and synaptic activity to alter pain behavior within minutes to tens of minutes after treatment with microglial activators and inhibitors.
What Happens If Microglia Are Damaged?
Inflammation may start to kill healthy brain cells, however, if it persists for a long period. Neurodegenerative conditions including Alzheimer's disease, Parkinson's disease, and Amyotrophic Lateral Sclerosis have all been linked to unchecked inflammation in the brain brought on by microglia.
Conclusion
The inflammatory response and the activation of microglia have been related to a number of neurodegenerative disorders, including Alzheimer's disease, Parkinson's disease, and frontotemporal dementia (FTD).
In order to have a complete understanding of the complex ways in which cells interact with one another, the activation of microglia has to be investigated. According to the findings of study, the activation patterns of microglia in brain diseases seem to be reliant on both location and context.
These parameters have been investigated during the course of this research, and it is possible that they have an impact on the performance of microglia in brain-related conditions such as Alzheimer's disease and Parkinson's disease (PD).
The development and activation of a number of different PRRs is another essential component, in addition to the environment and cell interactions with microglial cells, which play crucial roles in the process.
The interaction of a number of PRRs and ligands illustrates the mosaic of different responses that might be produced by microglia. Because of the wide variety of these diseases, researching them is a formidable obstacle for medical researchers but also presents an opportunity to create new remedies.
Jump to
What Is The Definition Of Neurological Disease?
What Is A Microglia?
Alzheimer’s Disease Pathology
Activation Of Microglia In Alzheimer’s Disease
Frontotemporal Dementia
Activation Of Microglia In Frontotemporal Dementia
Parkinson’s Disease
Activation Of Microglia In Parkinson’s Disease
Directions For The Future
People Also Ask
Conclusion

Karan Emery
Author

James Pierce
Reviewer
Latest Articles
Popular Articles