Behavioral And Psychological Symptoms Of Dementia - Its Causes And Management
Neuropsychiatric symptoms, sometimes referred to as behavioral and psychological symptoms of dementia (BPSD), are a wide variety of non-cognitive symptoms and behaviors that are seen in dementia patients.
Author:Katharine TateReviewer:Karan EmeryOct 10, 202324.3K Shares343.5K Views
Neuropsychiatric symptoms, sometimes referred to as behavioral and psychological symptoms of dementia(BPSD), are a wide variety of non-cognitive symptoms and behaviors that are seen in dementia patients.
BPSD stands for behavioral and psychological symptoms of dementia.
A diverse collection of clinical events, such as disordered emotions, mood, perception, thinking, motor activity, and personality features, are experienced subjectively by the patient and/or observable by an examiner as part of the natural progression of dementia.
These clinical events can be broken down into several categories (e.g., caregiver, physician).
According to the International Psychogeriatrics Association, these "neuropsychiatric symptoms," or behavioral and psychological symptoms of dementia, are extremely common.
They are also associated with high levels of distress in both dementia patients and caregivers, as well as adverse outcomes and increased utilization of healthcare resources.
In addition to cognitive impairment, BPSD is thus a potential and major therapeutic target for the treatment of the condition.
BPSD In The Current Classification System
Although BPSD is almost always present in dementia, it is not taken into account by the diagnostic procedures that are now in use.
Both the DSM-IV-TR and the ICD-10 define dementia as the progressive emergence of a number of cognitive impairments (including memory and at least one other cognitive domain), which do not occur solely during delirium and constitute a deterioration in functioning.
Dementia is defined as a progressive emergence of multiple cognitive impairments (including memory and at least one other cognitive domain).
The DSM-IV-TR has a coding system that indicates the presence or absence of clinically relevant behavioral abnormalities but does not provide diagnostic criteria.
To better describe the clinical characteristics of dementia, it is also possible to classify dementia (such as Alzheimer disease, AD) in axis III and some mental disorders (such as mood or psychotic disorder) in axis I.
This would allow for a more precise classification of dementia.
Psychopathological Features
Dementia is characterized by a wide variety of unpredictable neuropsychiatric symptoms, which may have an effect on a person's mood, reasoning, perception, and motor function.
Although the clinical presentation of dementia may vary greatly across different pathology subtypes and even between individual dementia patients, there are certain symptoms that are more prevalent in particular pathology subtypes.
To begin, diagnose and explain the psychopathology, then differentiate between symptoms that are similar in order to have a better understanding of the mental manifestations of dementia (e.g., depression vs. apathy).
This is tough to do since symptoms tend to overlap and there is a lack of diagnostic criteria and definitions.
Second, it is useful to examine whether or not certain symptoms occur together and combine them into syndromes that have comparable clinical development, neurobiology, and treatment options.

What is dementia?
Emotional Disruptions
The patient seldom displays grief, unhappiness, preoccupation with depressing matters, despair (associated to suicidal ideas), and loss of self-esteem since dementia often conceals depressive symptoms.
The three main symptoms of an anxiety disorder are anhedonia (loss of interest in once pleasurable stimuli), physical issues, and anxiety (a subjective unpleasant sensation of dread shown as apprehension, tension, panic, or worry).
In dementia, apathy is a motivational disorder marked by diminished goal-directed activities, cognitive functions, and emotions. Loss of interest, sluggishness, and exhaustion are symptoms shared by both apathy and depression. Apathy is a lack of motivation without pain.
From hypomania to severe mania, an elated mood is characterized by a persistent, overwhelming feeling of happiness, joy, or euphoria that is out of proportion to the situation.
Usually, it's accompanied with an emotionally charged tone or reaction.
A continuous feeling of unease in response to a threat that may be exacerbated by hunger, tiredness, and discomfort is associated with both grief and elation.
Affective lability is indicated by sharp mood shifts within seconds or minutes.
Delusions And Abnormal Thinking
The level of complexity, systematization, conviction, and the extent to which patients act on their delusions to varying degrees are all characteristics of delusional thinking.
Delusions are characterized by suspiciousness, abandonment, and misidentification, and they are less intricate and orderly than those that are experienced by non-demented psychotic persons.
Examples of common Capgras delusions include the conviction that: people are coming into the home and hiding or stealing objects; the place one is residing is not one's home; the conviction that one's spouse is an impostor (Capgras delusion); the accusation of a conspiracy to abandon or institutionalize; the conviction that one's spouse is unfaithful; the belief that others have acted maliciously or with discriminatory intent.
The feelings of guilt, worthlessness, reference, and persecuting others may be associated with illusions brought on by depression.
Perceptual Disturbances
All of a person's senses might be affected by dementia.
When there are no external sensory inputs present, it might be difficult to determine if a patient's perceptual disturbance is an illusion or a sense of what is happening (hallucination).
Patients suffering from Lewy body dementia often have hallucinations of the visual kind. Images, either of people or animals, that appear repeatedly and are described in great detail by the patient.
Disturbances To Motor Function
Problems with motor function may be instantly identifiable as decreased or increased motor activity; specific motor abnormalities are not required for this diagnosis.
Motor retardation is characterized by delayed movements and speech, decreased body tone, and a reduction in the number of spontaneous body movements.
Increased energy, frequent movement, and/or rapid speech are some of the characteristics of the neurological disorder known as motor hyperactivity.
Agitation is defined as "verbal, vocal, or physical conduct that is improper and does not arise directly from the demands or confusion of the one who is agitated."
This term is used interchangeably with aberrant motor behavior and encompasses actions such as walking away from home, recurrent, purposeless acts, and socially unacceptable activities such as disinhibition.
In addition, aberrant motor behavior may be defined as abnormal movement patterns (a tendency to disregard social and cultural norms and not restrain inner feelings, such as sexual drives).
Cohen-Mansfield (1999) classified agitation as falling into one of four categories: vocally non-aggressive; physically non-aggressive; physically aggressive; and verbally aggressive.
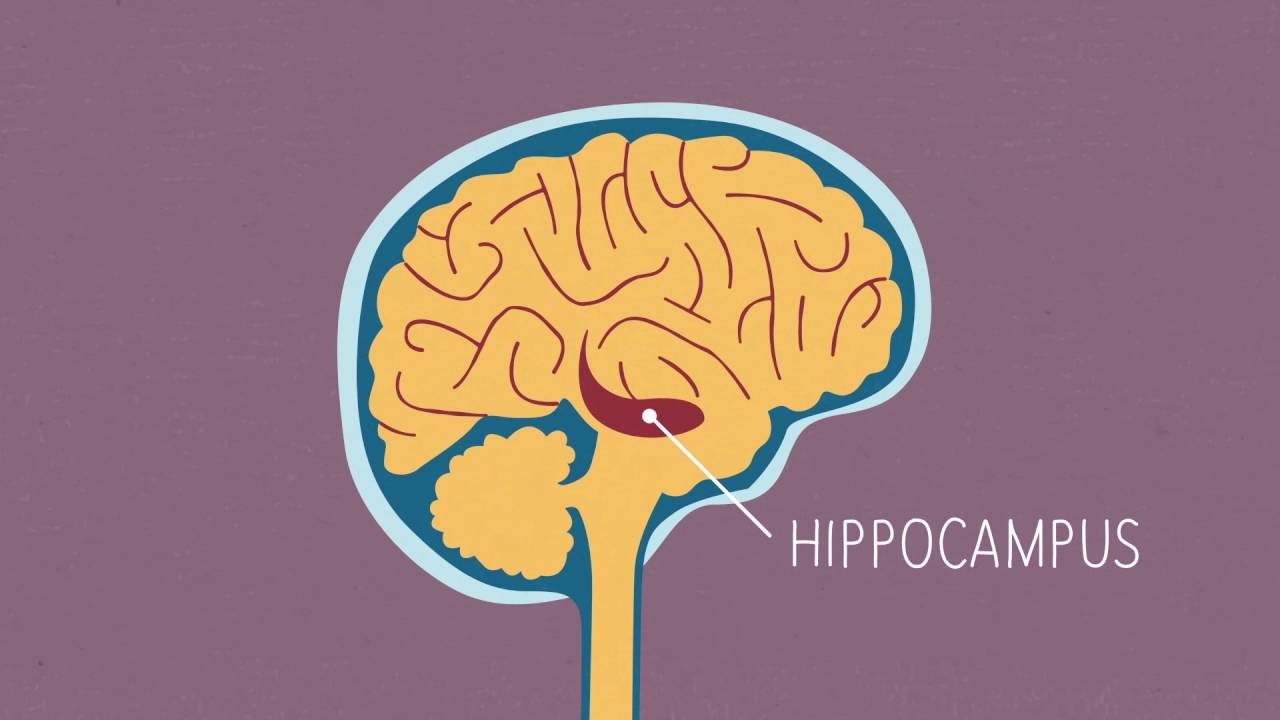
What is dementia? Alzheimer's Research UK
Circadian Rhythms
Alterations in sleep patterns are a typical part of the aging process, although dementia is becoming increasingly prevalent as people become older.
Insomnia, hypersomnia, sleep-wake cycle reversal, fragmented sleep, and rapid eye movement sleep behavior disorder are some of the conditions that fall under this category.
Naps throughout the day and awakenings in the middle of the night are typical behaviors seen in dementia patients.
There is a possibility that pain, the need to urinate throughout the night, some medications (diuretics), and stimulants such as coffee and bronchodilators are all contributors.
Appetite And Patterns Of Food Intake
Examples of quantitative and qualitative changes in appetite include anorexia and hyperphagia, respectively (preference for particular foods associated or not with changes in taste).
The desire for sugary foods is quite common among those who have frontotemporal dementia.
The majority of people who suffer from dementia have weight loss, which may be caused by hormonal imbalances, hypermetabolism, or inflammatory processes.
The Neurobiology And Pathophysiology Of BPSD
Disorders of behavior or psychology that are associated with dementia are attempts to cope with environmental or physiological stress that are ineffective.
BPSD is also common in older people who do not have dementia, with rates of 5.6 percent for anxiety, 4.5 percent for irritability, and 2.8 percent for agitation/aggression.
On the other hand, 10.5 percent of Swedish 85-year-olds showed psychotic symptoms. Constitutional factors (such as personality) characteristics, cognitive styles, and emotional reactivity), past experiences, and level of education all have an impact on premorbid psychosocial performance.
Abnormalities in internal conditions and/or visible behaviors are likely to develop beyond the usual variability when a person has dementia because the neuropathological changes of dementia influence the individual's psychological capability to adjust to day-to-day demands.
The area of research that aims to define the neuroanatomical and neurochemical correlates of BPSD in order to design treatments that are more successful is one that is still active.
Management Of BPSD
In order to control BPSD effectively, a strategic combination of pharmaceutical and non-pharmacological treatments is required.
Because there is a risk of excessive use of psychotropic medication, clinical practitioners have difficulties managing these symptoms effectively.
According to the most recent recommendations, non-pharmacological therapies should be attempted first, followed by the use of the drug with the lowest risk for the shortest amount of time.
Non-Pharmacological Interventions
Cognitive and emotional therapies, such as reminiscence therapy, simulated presence therapy, and validation therapy, as well as sensory therapies, such as acupuncture, aromatherapy, light therapy, massage/touch, music therapy, Snoezelen multisensory stimulation, and transcutaneous electrical nerve stimulation, fall under the category of non-pharmacological interventions.
Other psychosocial and behavioral therapies also fall into this category. In spite of efforts to research these tactics, there is not sufficient data to support claims that they are successful.
Individual psycho-educational therapy provides caregivers with long-term advantages that are beneficial in the long run.
Since the 1980s, nursing homes and other types of long-term care institutions have had specialized care units.
A trained staff, a personalized atmosphere, and active participation from the family are all qualities.
Pharmacological Interventions
BPSD is treated with antipsychotics, antidepressants, anticonvulsant mood stabilizers, ChEI, benzodiazepines, and memantine.
These medications' efficacy in treating BPSD varies by symptom and class.
The pharmacological therapy of BPSD should address comorbidities and accompanying drugs that enhance medical problems and drug interactions.
Current recommendations propose weighing the advantages and risks of each drug class and using the least damaging medicine for the shortest period feasible.
Antipsychotics
Antipsychotic medication has been more popular ever since the introduction of atypical antipsychotics.
They provide treatment for aggressive behavior, psychosis, and agitation. The validity of the other BPSD symptoms is questionable.
Off-label use of antipsychotic medications is common despite the fact that they may cause dangerous side effects, including extrapyramidal symptoms, sleepiness, tardive dyskinesia, gait problems, falls, anticholinergic side effects, cerebrovascular events, and increased mortality.
Risperidone, olanzapine, and haloperidol assist in controlling BPSD.
According to studies conducted on people with dementia, haloperidol was associated with a mortality rate that was 1.5 times higher than that of risperidone, olanzapine, or quetiapine.
The risk of death caused by haloperidol was highest during the first month of treatment and gradually decreased after that.
Antipsychotic medication should only be used for short periods of time to treat severe symptoms such as agitation, aggression, and psychosis.
This is because of the increased risk of having a stroke or passing away from these conditions.

Antidepressants
For older BPSD patients, antidepressants may be an efficient and well-tolerated substitute for antipsychotics.
Several members of this drug family, especially selective serotonin reuptake inhibitors (SSRIs), are used to treat depression.
Citalopram and sertraline were just as successful in treating agitation and psychosis in dementia patients as haloperidol and risperidone, but they were also more tolerable and safe.
Citalopram was used to treat disinhibition, anger, and depression brought on by FTD.
The evidence is against taking these medications for any BPSD other than depression.
Cholinergic Inhibitors
The recommendations for each drug are different; nonetheless, the current guidelines encourage the use of ChEI for BPSD.
There is only a marginal improvement in Alzheimer's disease symptoms after treatment with donepezil, galantamine, or rivastigmine.
ChEIs reduce the severity of behavioral changes and slow down or stop the degradation of cognitive and functional abilities.
ChEIs have the potential to treat symptoms such as apathy, depression, and aberrant motor behavior.
Memantine
The NMDA receptor antagonist, memantine, may enhance behavior, cognition, and function, but there is insufficient evidence to recommend its use.
Memantine appears to benefit certain habits, such as impatience and anxiety (mood symptoms, apathy, and aberrant motor behavior).
Patients with several BPSDs may benefit from combined therapy.
The most recent evidence on combination memantine and ChEIs (donepezil) treatment indicated only a little increase in NPI ratings and no appreciable improvements in cognitive and behavioral changes in people with moderate-to-severe AD.
Anticonvulsants
Anticonvulsant mood stabilizers such as carbamazepine, valproic acid, gabapentin, lamotrigine, and topiramate are often used in clinical practice.
Some dementia patients find mood stabilizers to be helpful.
Although studies on the benefits, safety, and tolerance of anticonvulsants have shown mixed results, it is possible that they might help reduce the dose of antipsychotics. Sodium valproate has been connected to falls, infections, and GI problems in addition to being ineffective at managing AD agitation.
Benzodiazepines
The use of benzodiazepines as a short-term therapy option is something that might be considered in situations involving acute agitation or agitation brought on by anxiety.
People Also Ask
Which Of The Following Is A Psychological Symptom Of Dementia?
Agitation, despair, apathy, persistent questioning, psychosis, violence, sleep issues, roaming, and other inappropriate behaviors are some of the behavioral and psychological signs of dementia. Nearly all dementia patients will experience one or more of these symptoms during the course of their condition.
What Is Challenging Behavior In Dementia?
Shouting, roaming, biting, throwing items, repetitive speech, trashing personal belongings and other objects, agitation and general rage, physical assaults on others, and keeping people up at night are all examples of challenging behavior in the setting of dementia.
How Does Dementia Cause Feelings And Behaviors?
People who have dementia may repeatedly express or ask the same questions.
Additionally, they could grow too attached to you and follow you everywhere, even to the bathroom.
These actions may be quite distressing and grating.
What Is An Effective Behavioral Intervention For Dementia?
It is possible to minimize agitation and other problematic behaviors in people with dementia via person-centered care and communication, sensory stimulation, and listening to music.
Conclusion
Dementia patients often exhibit neuropsychiatric symptoms, which may cause significant stress for caregivers and medical costs.
The correct identification and evaluation of these symptoms is an important component of the clinical approach to dementia.
To date, no standardized model has been developed despite early efforts to group various symptoms (in order to facilitate clinical/diagnostic investigations).
There is no established cause for these symptoms, although current research suggests many possibilities.
New research methodologies may help us better grasp the underlying causes of many neuropsychiatric conditions.
Therapy for BPSD is currently the best combination of non-pharmacological and appropriate pharmaceutical methods.
However, there is no reliable evidence to support the use of specific treatment approaches for different types of symptoms.
Emerging non-pharmacological approaches that are safer than pharmaceutical treatments must be promoted aggressively.
More research is also needed to find pharmacological treatments that are more effective, safe, and well-tolerated.
A better understanding of BPSD symptoms in dementia patients will assist in the creation of new, more symptom-focused, and precise therapeutics.

Katharine Tate
Author

Karan Emery
Reviewer
Latest Articles
Popular Articles